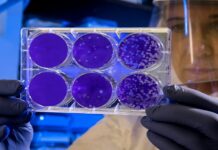
Cancer therapies often have short-lived benefits due to the emergence of genetic mutations that cause drug resistance. A key gene that determines resistance to a range of cancer drugs has been reported in a study published by Cell Press November 21st in the journal Cell. The study reveals a biomarker that can predict responses to cancer drugs and offers a strategy to treat drug-resistant tumors based on their genetic signature.
“We need to understand the mechanisms of drug resistance to effectively prevent it from occurring in the first place,” says senior study author René Bernards of the Netherlands Cancer Institute. “We have identified a mechanism of drug resistance that is caused by the activation of a specific signaling pathway in cancer cells.”
Non-small cell lung cancer (NSCLC) is the most common type of lung cancer, and NSCLC patients with a specific type of tumor mutation can be treated with a targeted therapy called crizotinib. But these patients frequently develop drug resistance as a result of secondary mutations in their tumors, through unknown genetic mechanisms.
To gain insight into this question, Bernards and his team developed a screen to identify genes whose suppression confers resistance to crizotinib in NSCLC cells. They discovered that inhibition of MED12, a gene that is mutated in cancers, resulted in resistance to not only crizotinib, but also other targeted drugs and chemotherapy used to treat various types of cancer.
The researchers also found that MED12 suppression caused drug resistance by enhancing signaling through the transforming growth factor beta receptor (TGF-betaR) – a protein involved in cell growth and cell death. By inhibiting TGF-betaR signaling in MED12-deficient cells, they were able to restore drug responsiveness. The results suggest that TGF-betaR inhibitors, which are currently being tested in clinical trials, may counter drug resistance in cancer patients with MED12 mutations.